
One of the tragic consequences of COVID-19 vaccination I have come across is the rapid onset of (often fatal) dementia in elderly individuals. Because the elderly often lack the ability to advocate for themselves and are no longer considered a priority by our society, these deaths have been quite easy to sweep under the rug (it is not well known, but many of our elders needlessly died throughout the pandemic).
I would argue that our priorities should change as most of us will eventually end up in the same situation currently faced by our elders. Additionally, I would argue that many of the complications of aging are not natural and instead reflect the cumulative effect of unhealthy practices conducted throughout society, particularly within the profit-driven field of medicine.
One of the most challenging diseases of aging is Alzheimer's disease. Despite over a century of research and billions being spent on Alzheimer's disease research (3.1 billion was allotted for Alzheimer's and dementia research in 2021), cures for this disease remain elusive (the existing treatments have a negligible benefit but incur significant side effects) and the costs for it keep rising (last year Alzheimer's was estimated to cost the United States 355 billion dollars).
Given the enormous economic and social cost of Alzheimer's disease (which any of you will understand if you have a relative with Alzheimer's), one must ask why no treatment has ever been found for it. The answer is quite simple: multiple effective therapies have been found, but each lies outside the currently accepted paradigm. So, rather than consider these approaches, the focus has instead been on desperately attempting to find a solution within the current paradigm, and it is my hope the previously cited figures illustrate the absurdity of continuing this approach.
The Amyloid Hypothesis
The existing dogma within Alzheimer's research is that Alzheimer's disease results from the buildup of amyloid plaques within the brain which then cause brain damage that leads to Alzheimer's disease. The majority of research for treating Alzheimer's disease has thus been targeted at eliminating these plaques:
Hundreds of clinical trials of amyloid-targeted therapies have yielded few glimmers of promise, however; only the underwhelming Aduhelm has gained FDA approval. Yet Aβ still dominates research and drug development. NIH spent about $1.6 billion on projects that mention amyloids in this fiscal year, about half its overall Alzheimer’s funding. Scientists who advance other potential Alzheimer’s causes, such as immune dysfunction or inflammation, complain they have been sidelined by the “amyloid mafia.” Forsayeth says the amyloid hypothesis became “the scientific equivalent of the Ptolemaic model of the Solar System,” in which the Sun and planets rotate around Earth.
Note: The approval for Aduhelm was immensely controversial, as ten of the eleven members of the FDA panel voted against approving it, and three resigned following it nonetheless being approved. The drug, priced at $56,000 a year (and therefore capable of bankrupting Medicare), failed to show any improvement for Alzheimer's disease while brain swelling or brain bleeding was found in 41% of patients enrolled in its studies. There also appears to have been inappropriate relationships within the FDA that led to Aduhelm receiving an accelerated approval (which like the vaccine emergency use authorizations allowed certain requirements that would have otherwise needed to be met to bring the product to the market to being waived).
I would thus argue the amyloid hypothesis has not been the best area to focus upon. Unfortunately, as I learned early in life, any business which depends on solving a problem will never solve the problem because it has an inherent self-interest in not doing so (as that would terminate its support). This holds true both for many areas of medical research and also throughout our society.
The rigid adherence to the amyloid hypothesis underscores two key problems within medicine: the shortcomings of a reductionistic model for chronic diseases and how easy it is to guide the direction of the scientific literature.
Reductionism
Nature is immensely complicated, so to navigate it, human beings always must make models to simplify it into something that can be understood (typically through reductionism—understanding something through breaking it into its smallest parts). In some cases, these models work extraordinarily well, but in many other areas, they abjectly fail. In the context of medicine, I often find that acute conditions respond well to a reductionistic framework, but in most cases that model fails abjectly for chronic conditions (hence why they remain chronic).
In a recent article, I sought out the advice of mentors for an explanation as to why doctors aggressively push dangerous medicines on their patients. One of the most common answers I received was that the entire therapeutic base of modern medicine relies upon prescribing pharmaceutical drugs. Following this model in turn requires each adherent to have faith a pharmaceutical silver bullet can be found for a disease (which does sometimes happen), and as a result, my profession has not been able to let go of the hope of that targeting the amyloid plaques will be that silver bullet.
In most cases, chronic diseases either arise from an unresolved problem few practitioners can even identify (which often is a pharmaceutical side effect), or from an inertia being created towards a state of ill health that was never corrected and allowed to compound until it became solidified within the body. Put differently, many chronic diseases represent a natural process that has gone awry and never was corrected; by the time we try to intervene in them, they have built up so much inertia that it is difficult to directly oppose their progression with the tools available to each physician.
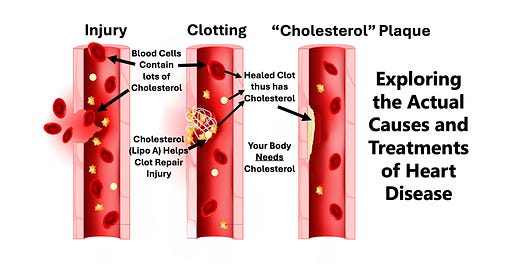
One of the best examples I have seen in this subject relates to heart disease, which remains the top cause of death in America despite enormous amounts of resources being directed towards it for decades. Many authors have made the case that contrary to widely held belief, cholesterol does not cause heart disease, and that cholesterol management (e.g. with statins) has significant harms with minimal to no benefit (I wholeheartedly agree with this assessment).
One of the best models I have come across for explaining the cause of heart disease (there are other important models I will also discuss in the future), comes from my favorite cholesterol skeptic, Dr. Malcolm Kendrick. He has provided conclusive evidence that demonstrates the vascular damage which creates heart disease is a result of repeated blood clots forming upon damaged vasculature and has nothing to do with blood cholesterol levels.
Kendrick’s point that a common chronic disease is often the manifestation of a maladaptive but normal physiologic process is critical for understanding many chronic diseases including Alzheimer's. Unfortunately, medical practitioners often have a great deal of difficulty observing how a small problem can smolder in the background until it eventually becomes entrenched within the body and causes serious disease, or how one unaddressed physiologic distortion can grow and grow until it completely distorts the natural functions of the body. Effective natural medical systems in contrast recognize this and seek to gradually reverse those physiologic processes until a normal physiology and a reversal of the chronic disease is arrived at.
Kendrick’s point is important, because, in addition to applying to heart disease, it also holds equally true for the development of Alzheimer's disease.
Peer Reviewed Orthodoxy
One of the common objections raised against “peer reviewed" literature is that the peer review process is highly political and primarily serves as a filter to ensure only papers matching the prevailing biases of medicine (or industry interests) become published within the scientific literature. Most commonly, this is demonstrated by papers that match the prevailing biases of medicine being held to a very low editorial standard, whereas papers that conflict with those biases are held to nearly impossible-to-meet standards.
This, I believe, is why the Lancet recently published a misleading presentation of V-safe’s data which was then used to claim this database indicated the vaccines were safe when it in fact showed the opposite , and another large study which erroneously claimed hydroxychloroquine was deadly that relied upon a clearly fraudulent database that eventually resulted in the retraction of the paper. Because of this bias, most papers that unearth controversial data will typically claim the opposite of what their data suggests in both their summary and conclusion in order to have a chance of passing peer review and being published.
Another major issue with the peer reviewed literature is that once an “authority” becomes established within a field, other authors are hesitant to challenge that authority, and will instead publish papers that agree with the author’s conclusions so that they can also pass peer review.
Note: A major reason why I have so much respect for Paul Marik (a widely acclaimed critical care doctor who was recently fired and blacklisted for refusing to kill his patients by following the government COVID-19 protocol) is because throughout his career, Marik has saved many lives by debunking unsubstantiated beliefs throughout the critical care literature. Unfortunately, doctors like Marik are the exception rather than the norm, and as the years go by, it is harder and harder for them to practice within the corporatized field of medicine, which requires every doctor to follow a rigid treatment algorithm that often does not address the needs of their individual patient.
In the case of the amyloid hypothesis, a similar bias has also infested the peer review literature.
Amyloid Research
The early history of Alzheimer's research is as follows: In 1906, plaques in the brain were identified as the cause of Alzheimer's disease, in 1984, amyloid beta protein was identified as the primary component of those plaques, and in 1991, genetic mutations in a protein that gives rise to amyloid beta was linked to inherited forms of Alzheimer's disease.
Although these discoveries provided hope that a cure for Alzheimer's was at hand, the abject failure of this model to produce a meaningful benefit (there are hundreds of failed clinical trials that targeted amyloid beta) gradually attracted a large group of skeptics towards it. They instead investigated many other factors that appeared to play a much more significant role in causing the disease (e.g. chronic inflammation), and by 2006, this perspective appeared poised to change the direction of Alzheimer's research.
Frequently when a faulty paradigm fails to explain the disease it is claims to address, rather than admit the paradigm is flawed, its adherents will label each conflicting piece of evidence as a paradox (e.g. the French "paradox" clearly disproves the cholesterol hypothesis) and dig deeper and deeper until they can find something to continue propping up their ideology. Although I disagree with the perspective that viruses do not exist, I do agree with its adherent’s argument that profound scientific distortions or misinterpretation can underlie axioms within medicine and that it is often necessary to critically appraise the axiomatic beliefs in our profession (the amyloid saga is a perfect example).
One purported explanation by its proponents for the shortcomings of the amyloid hypothesis was that the cause of Alzheimer’s was not from amyloid plaques in general, but rather with certain toxic oligomers (smaller clumps of amyloid beta). In 2006, as dissent towards the amyloid hypothesis was reaching a critical mass, a paper published in Nature identified a previously unknown toxic oligomer, amyloid beta star 56 or Aβ*56, and provided proof it caused dementia in rats.
This paper cemented both the amyloid beta and toxic oligomer hypotheses (as it provided the proof many adherents to the theory had been waiting for) and rapidly became one of the most cited works in the field of Alzheimer's research. Its authors rose to academic stardom, produced further papers validating their initial hypothesis, and billions more were invested by both the NIH and pharmaceutical industry in research of the amyloid and toxic oligomer hypothesis.
It should be noted that some were skeptical of their findings and likewise were unable to replicate this data, but rarely had a voice in the debate:
The spotty evidence that Aβ*56 plays a role in Alzheimer’s had [long] raised eyebrows. Wilcock has long doubted studies that claim to use “purified” Aβ*56. Such oligomers are notoriously unstable, converting to other oligomer types spontaneously. Multiple types can be present in a sample even after purification efforts, making it hard to say any cognitive effects are due to Aβ*56 alone, she notes—assuming it exists. In fact, Wilcock and others say, several labs have tried and failed to find Aβ*56, although few have published those findings. Journals are often uninterested in negative results, and researchers can be reluctant to contradict a famous investigator.
The Amyloid Scandal
Near the end of 2021, a neuroscientist physician was hired by investors to evaluate an experimental Alzheimer's drug and discovered signs its data consisted of doctored images of Western Blot protein tests (and therefore erroneous assessments of what oligomers were present within research subjects’ brains). As he explored the subject further, he discovered other papers within the Alzheimer's literature had been flagged by Pubpeer (a website scientists use to identify suspect studies) for containing doctored Western Blots.
Before long, he noticed three of these papers had been published by the same author and decided to investigate their other publications. This led him to the seminal 2006 Alzheimer’s publication, which like the author’s other works contained clear signs of fraud (note: one of the most common reasons why criminals get caught is because they repeatedly commit the same crime—humans after all are creatures of habit). In short, these findings suggested the presence of the infamous Aβ*56 may have actually been a result of doctoring the Western Blot to support the author’s desired conclusion.
A subsequent investigation uncovered 20 papers written by the author, 10 of which pertained to Aβ*56, Many outside investigators agreed that the images had been doctored and a co-researcher came forward stating he had previously suspected the author of scientific misconduct and withdrawn his collaboration with the author for that reason. Despite being notified of this investigation, the suspect author was nonetheless awarded a coveted research grant by the NIH (which was signed off by another one of the authors of the 2006 paper) and the author remains employed by the University of Minnesota medical school.
As far as I can gather, the scientific community has been hesitant to directly condemn the author’s findings (as I believe he created a "too big to fail” situation). Thus far, notices of possible data integrity issues have been placed on some of his publications, and a gradual investigation has been launched of his findings which may eventually result in something being done.
In reviewing the saga, I find it interesting to consider how many forces will conspire to support a medical dogma once a sufficient financial and reputational investment has been made into it. In many ways, this process is identical to what occurs within the body as the process of a chronic disease establishes itself within normal physiology, and sadly is just as difficult to address.
Conclusion
One of the most noteworthy lines from the summary of this saga was:
“You can cheat to get a paper. You can cheat to get a degree. You can cheat to get a grant. You can’t cheat to cure a disease,” he says. “Biology doesn’t care.”
In many ways, the same could be said for the disastrous pandemic response and the fraudulent data provided to justify vaccine mandates across the globe.
As a result of the market forces that support the present medical monopoly and the collective conditioning physicians received to gaslight patients with pharmaceutical injuries, an ineffective therapeutic with significant adverse effects can frequently remain on the market. However, because of how extreme the risk-to-benefit ratio is for the COVID-19 vaccinations, this issue has, at last, become apparent to the general public. Remember, although propaganda is remarkably effective at controlling the minds of the populace, it is not yet sophisticated enough to consistently make its subject deny their direct experience.
No amount of propaganda can change the mind of someone who directly witnessed multiple severe vaccine injuries in their immediate circle and linked the events together. For this reason, although it is worrisome that we have had to pay a severe price for the COVID-19 vaccination campaign, I am very hopeful we are now entering an era where biology at last will hold doctors (and regulators) accountable for the medications they prescribe.
Thank you so much for reading the first part in this series. Please consider sharing this article with the appropriate audiences (e.g. Gab or GETTR), as I know this is an issue that affects many of our families. In the next part, we will look at what I believe causes Alzheimer's disease as the foundation for doing so has at last been laid out in this substack. The entire process is fascinating and provides many valuable insights for treating the disease (effective treatments for Alzheimer’s do in fact exist).









Once again, thank you for your writings. This one hits close to home. I’ve seen numerous cases of dementia getting much worse in the elderly after the mRNA shot. It’s so sad…families refuse to see the causation. In one case close to me, the 90yo man, who was brilliant and still at it one year ago, has gone downhill so fast, it’s shocking. My experiences with BP meds for a few months 20+yrs ago, and a short stint (no pun intended lol) on statins after a cardiac scare in early 2020 after what we think was very early case of covid, have opened my eyes to the issues with pharmaceuticals. The book “The Great Cholesterol Myth” played a big part in that eye opening. Getting off sugar and refined carbs, exercise and taking the supplements recommended has transformed me. Lost weight and normal BP now. That said, I’m pretty discouraged with our current medical establishment… I wish you were my Doctor.
The short answer of why we can't cure Alzheimer's: fraud.
Fraud on every level. Criminal fraud.