Since I no longer have the time to respond to all the correspondences I want to respond to, I began doing monthly open threads where I could focus on addressing the remaining questions that had accumulated over the last month, and tagging each open thread to a topic I have wanted to write about but didn’t feel quite merited its own article.
In this month’s open thread, I’ll share my thoughts on a question many have asked me since Trump and RFK Jr. won the election and an actual window has been created to change healthcare policies in America—what could be done to increase the survival rates in our hospitals and how can you protect a loved one that’s hospitalized?
This question, in turn, is a reflection of a sobering realization many had throughout COVID-19—what many of us believed about our hospitals was utterly incorrect, and rather than help patients, hospitals effectively functioned like assembly lines that ran disastrous protocols (e.g., remdesivir), denied patients access to their loved ones and refused to use alternative therapies (e.g., ivermectin) even when it was known the patients were expected to die otherwise.
For example, during COVID-19, one travel nurse who was assigned to a New York hospital with one of the highest death tolls in the nation realized something very wrong was happening throughout the hospital and decided to covertly record her colleagues and become a whistleblower
Within her testimony, one particular recording she made was particularly illuminating as a doctor perfectly illustrated the dysfunctional mentality that has infected our medical system by stating he was unwilling to try any alternative therapy (which had some evidence behind it) for patients he knew would otherwise die.
Much of this in turn, was due to a series of standardized treatment protocols being created for COVID-19, which heavily financially incentivized remdesivir and then ventilator care while simultaneously avoiding an effective off-patent treatment for COVID-19. Despite remdesivir actually increasing the death rate from COVID-19, hospital administrators still pushed their doctors to use it (and retaliated against those who did not follow the NIH COVID protocols) because of how powerful the financial incentives were for doing so.
Note: the NIH COVID treatment panel continued to make remdesivir the standard of care for COVID-19 and forbid alternative therapies (e.g., ivermectin) even as a mountain of evidence piled up that argued against it. This was due to Anthony Fauci appointing the committee and selecting chairs that had direct financial ties to Remdesivir’s manufacturer—an issue that sadly holds true for many other committees which create the guidelines that dictate medical care in the United States (e.g., in a previous article I showed how America’s cholesterol guidelines were authored by individuals taking money from statin manufacturers and that the conclusions those panels reached were the exact opposite of an independent one which evaluated the same data).
Overall, the remarkable illustration of this corruption was the fact that families eventually began suing hospitals to allow the use of ivermectin for a relative who was expected to die even after being subjected to Fauci’s hospital COVID protocols. Remarkably, because there was so much money on the line, the hospitals chose to fight these lawsuits in court rather than just give ivermectin to the patients. In turn, of the 80 lawsuits filed by lawyer Ralph Lorigo, in 40 the judge sided with the family, and in 40 with the hospital, and of those, in the 40 where patients received ivermectin, 38 survived, whereas of the 40 who did not, 2 survived—in essence making suing a hospital arguably the most effective medical intervention in history. Yet, rather than take this data into consideration, the profit-focused hospitals banded together to develop an effective apparatus to dismiss further lawsuits.
As I had expected something like this to happen, shortly before the pandemic, I put into place a plan to treat people at home (e.g., by procuring high-powered oxygen concentrators with non-invasive ventilation) and subsequently had numerous people in my immediate circle who we successfully treated at home, whom I am almost certain given their condition would have immediately been hospitalized and likely die at the hospital.
Note: this approach built upon the fact prior to COVID, we had other patients we felt merited a hospitalization but simultaneously expected to be put on the palliative care pipeline once admitted, so we’d learned how to provide a significant amount of the care you’d receive in a hospital at home, alongside the integrative therapies that were highly likely to actually help the patients recover.
Likewise, I also heard of more stories than I can count throughout the pandemic where a relative snuck an “unapproved” therapy to a patient in the hospital, which in turn saved the patient’s life, and a few cases where a doctor who was hospitalized needed to change their own treatment (while the nurses were gone) because no one would listen to the rationalizations they provided for optimizing their care.
Sadly, while this is quite depressing, it’s simply illustrative of a few more toxic trends that have taken over medicine.
Reductionist Realities
Anytime something happens, there are two aspects to it—the concrete variables of the situation and the intangible process that exists between those variables. Typically, modern science and academia focus on controlling and optimizing the concrete variables, while the essence of the phenomenon and its greater whole gets cast aside.
In turn, those who can nonetheless attain proficiency in those intangible areas end up excelling in their fields and rising to the top, because few can learn an art within a reductionist system that actively works against anyone developing those capacities.
In medicine, this dichotomy is illustrated by the contrast between the algorithmic version of medicine (where physicians are trained to rapidly execute precise protocols for each patient) and the art of medicine, where physicians constantly question each aspect of a patient’s care and take the time to both develop the plan that makes sense for the patient and foster each of the intangible aspects of the doctor-patient relationship which often bring about healing.
Sadly, as the years have gone by, medical training has shifted more and more away from teaching doctors how to treat patients and more and more to following treatment guidelines their corporate employers will expect them to implement, rather than independent practitioners whose clinical opinions were valued by the hospitals they worked in.
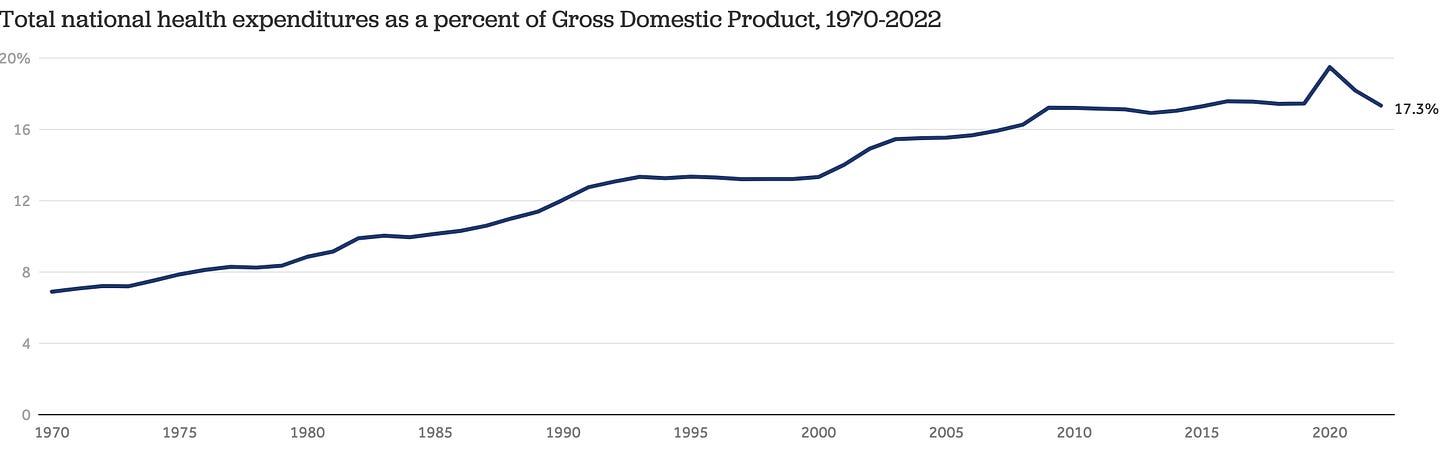
In tandem with this, the costs of healthcare in America have ballooned
Note: healthcare spending at the beginning of the 20th century was 0.25% of GDP, reached 1% in 1933, dropped to 0.38% during World War II, and went back up to 1% in 1961 before experiencing the meteoric rise it has seen in recent decades.
Most remarkably, despite spending 2-4 times as much on healthcare as any other affluent nation, the United States has the worst healthcare outcomes amongst the affluent nations (which is detailed within these charts). This I would argue, is a result of our healthcare spending prioritizing what corporate interests want, not what produces effective healthcare. Sadly, as I have shown in this article, pervasive corruption has entrenched itself throughout the Department of Health and Human Services and our healthcare officials.
As this costly trend is impossible to ignore, various proposals have been made to address it. Unfortunately, all of them have arisen from the same mentality that gave birth to the problem in the first place and thus have made it worse (e.g., creating more regulation to “improve” healthcare but having that regulation be created by bureaucrats who did not understand the realities of healthcare and shaped by corporate lobbyists who only care about profits).
Economic Enticements
In medicine, one of the most reliable means the government has to change the behavior of the healthcare system is by financially incentivizing the behavior they want (e.g., putting patients on remdesivir and then ventilators) since doctors and particularly healthcare workers will prioritize whatever the guidelines are regardless of what is in their patient’s best interests.
A key aspect of this process is the quality scores of hospitals graded on the quality of care they give patients (e.g., what percent of central lines become infected). In turn, some of these metrics are helpful, but many others are not (e.g., what percent of patients do you vaccinate). This is unfortunate because the rates at which Medicare reimburses hospitals (and then often other insurance providers) are set by how well they meet these metrics, so as a result, administrators will do everything they can to ensure hospitals do.
Note: much of this is mediated through JHACO. This non-profit organization assesses the quality of care hospitals provide, and hence their administrators put a great deal of effort into appeasing JHACO.
After age 40, the amount of money spent on healthcare increases exponentially, with 22% of all medical expenses (and 26% of Medicare expenses) being spent in the last year of life. Since there has always been a looming threat that Medicare will go bankrupt, reducing those expenses has long been a focus for healthcare bureaucrats (as best as I can gather, this began in 1979 but really kicked into gear with Obamacare).
Note: the individual that many of my colleagues believe was responsible for that shift was Ezekiel Emanuel, an oncologist and medical ethicist who was one of the chief architects of Obamacare (at which point he faced many accusations of promoting “death panels” which would deny costly care to people at the end of their lives) and later was placed on Biden’s COVID-19 advisory board.
Because each day you keep someone in an American hospital costs $2,883 (going as high as $4,181 in California) and strains the limited staffing resources, reducing hospital stays has always been a critical metric for healthcare bureaucrats. This in turn, has been accomplished by approaches such as:
•Giving hospitals a set fee for a patient admission rather than one dependent upon how many days they are in the hospital (which requires hospitals to eat (pay) the cost for a prolonged hospital stay).
•Having both JHACO and Medicare accreditation for critical access hospitals (which Medicare pays more to) be dependent upon the average length of hospital stay being 96 hours or less (as over that denotes “inferior care”).
As such, hospitals do everything they can to reduce the length of stay. This includes strongly pressuring doctors to shorten the length of stay, both through financial incentives for doing so and by reprimanding doctors whose patients stay too long (e.g., many hospitals have committees which identify “excessive” lengths of stays and then heckle the supervising doctor and require them to immediately provide a strong rationale for why the patient hasn’t been discharged).
Note: another major issue is that ER doctors have very different criteria for who they will admit to hospitals (e.g., some admit patients who are not very ill to avoid liability, while others only accept people who actually need hospital care). This creates a significant challenge on the hospital’s end both because it strains the limited hospital resources (by filling the beds—hence making the hospitals want to empty the beds as quickly as possible) and because it gives insurance programs an unrealistic expectation of how long patients require hospital care due to the less and more severe presentations of the same disease getting juxtaposed. together.
Time to Heal
Whenever a problem arises in medicine, the bureaucratic tendency is to find ways to micromanage the concrete variables at the expense of the intangible aspects of patient care. As such, almost all the protocols physicians are trained in (which are meant to improve the quality of medical care) tend to cast the intangibles to the side—to the point doctors are often penalized if they break from the protocols.
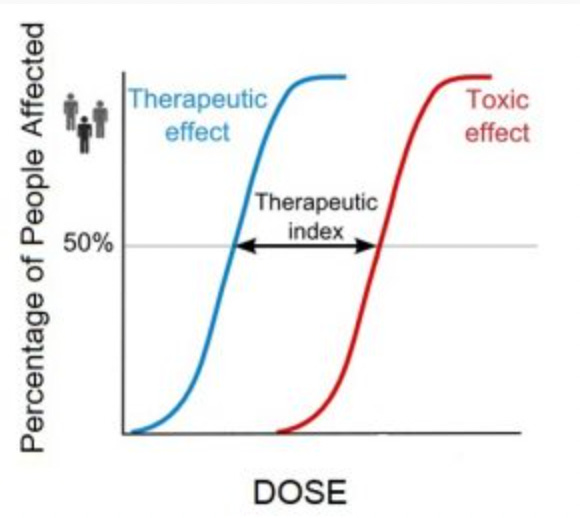
One area where this is particularly problematic is dosing, as different patients simply need different doses of the same therapy. For almost all therapies, a specific dose exists where most patients will begin to benefit from the therapy and another where they will begin to show toxicity.
In turn, doses are usually chosen by what’s in the middle of those two values (the therapeutic index). The problem with this is that since there is so much variation in patient’s sensitivity to interventions, what can be a therapeutic dose for one patient can instead be toxic for another. Since a standardized medical system can’t function without standardized doses, doses are used that frequently injure the more sensitive members of the population.
Note: the art of dosing and the methods we use to determine the correct dose for patients is discussed further here.
For instance, virtually every natural medicine system recognizes that “frail” patients typically cannot tolerate higher doses, and treating them correctly requires instead using a lower dose over a more extended period of time. Unfortunately, since hospitals are “required” to get patients out quickly, higher doses are used instead, which causes those with more robust constitutions (who can tolerate the therapies) to recover rapidly. In contrast, when those rapid protocols (that are designed to achieve a fast discharge) are used on the more frail patients, they do not respond well to them, and then once this happens, their family members are often told, “Nothing can be done for the patient”. They are pressured to send them to palliative care (e.g., morphine) or send them to hospice (e.g., they’re told the “unconscious” family member can never recover and would not want to live like this).
We believe this inappropriate dosing is a primary cause of unnecessary hospital deaths and that many “terminal” cases could recover with a slower course of treatment.
For example, in patients with congestive heart failure, a frequent scenario we’ll see is an aggressive diuretic regimen being done to get the excessive fluid out of their body. In more robust patients, this works and you can get them out within 2-3 days, but in weaker patients it can set off a variety of severe complications (e.g., low blood sodium or kidney failure). Good outcomes can only be achieved with a 4-5 day hospital stay and a gentle, well-paced diuresis (fluid draining) protocol.
Note: a similar issue happened during COVID with prematurely pulling patients off ventilators.
Because of these economic incentives, hospitals have gotten very efficient at moving patients through the palliative care pipeline, and hospital care often turns into a Darwinian situation where if you haven’t recovered in 3-4 days, you are ‘selected’ to pass away.
As such, hospitals are incentivized to “treat” patients with a standardized protocol rather than get them better. Many things that need to be done to improve patient outcomes simply are not done, and resources are inappropriately diverted.
For instance, hospitals routinely invest in social workers as they help to ensure patients can be discharged (e.g., by pressuring them). In contrast, nurses are so understaffed at hospitals that they often only have the time to take patients vital signs and give them the pills a doctor ordered, rather than examine each patient every few hours or become aware of what is ongoing with them (which is often critically important for positive health outcomes). The reality is that they should be evaluating patients every 2-3 hours.
Because of this, if slightly more money was spent to have 1-2 more nurses on each floor, it would be a relatively low-cost way to improve patient outcomes dramatically. In contrast, we believe the push to rapidly discharge patients from hospitals (e.g., with social workers) is ultimately quite costly to the medical system because when patients are sent out of the hospital without their health having been properly restored, they frequently will be readmitted numerous times.
In short, the current discharge criteria were created to “save” money by getting patients out of the hospital quickly (e.g., by sending them to a nursing home when they still have not fully recovered). Still in reality, since the “intangible” part of the healing process was cut out in the process, it actually ends up being far more costly to everyone involved because of how frequently those patients are later readmitted (particularly since multiple hospital admissions often give rise to a fatal downhill spiral for patients).
Consider for instance this email I received from a supporter of this newsletter:
"I formerly supported a health system’s Quality Analytics team (from both provider and insurer perspectives). I saw data for a lot of this—for example, showing that improving discharge planning discussions with caregivers, especially of older chronically ill patients, would reduce readmissions considerably. However, since that would require changing discharge protocols, no one was interested. :-("
Note: in contrast, accelerated hospital stays are much less of an issue for post-surgical patients because surgeons are financially penalized by the death rate for their patients within 30 days of surgery and hence incentivized to keep patients in the hospital for a sufficient length of time. This point helps to illustrate how many things in medicine result from economic incentives rather than what is best for a patient.
Training Priorities
This new paradigm is primarily a result of the younger doctors (particularly during their internship) being trained to execute protocols and request consultations rather than critically examine each case, explore what they are missing, and try to calibrate their treatment plan to each patient (e.g., in the past medical training had a much greater focus on adjusting doses). Most strikingly, doctors are trained to give up on patients and accept the inevitability of many illnesses, when in reality (with the correct approach) they are quite possible to treat.
To illustrate, I recently had a colleague who called me in tears because their father had been discharged to a hospice center, and was being started on palliative care because his case was terminal, but my colleague was convinced he was just dehydrated and needed saline. I asked, “Well you’re a doctor, can’t you get them to give the IV?” They said, “The nurses will only do it with the hospice physician’s authorization, so I need help.” We were eventually able to find a way to get him the IV (which made a big difference) but there was a roughly a four day delay in the process.
To an outsider, that situation seems a bit unbelievable, but in truth, it’s reflective of the current paradigm. As such, we believe a crucial aspect of “Making America Healthy Again” will be to change the training of hospital doctors (internists) across America so that they know how to provide the prolonged course of care patients need to get well and to remove the pressure to rapidly clear them out of the hospital and allow them to have the autonomy to do what they feel is best for their patients.
In contrast, our focus now instead is on optimizing palliative care. Sadly, many doctors don’t even know they are failing their patients because the current training is based on the expectation hospital stays should be 3-4 days, and they never lived in the era before these mandates where it was possible to see the benefits of more extended hospital stays.
Note: preventing hospital readmissions (especially for those who have entered the downhill spiral) often requires effective integrative medical care outside of hospitals (which unfortunately is another area where the current medical system does not train doctors).
Working With Your Hospital Doctor
Most individuals in the healthcare system recognize that some doctors get better results than others, and that to some extent, a patient’s survival is dependent upon who they work with and which hospital they go to.
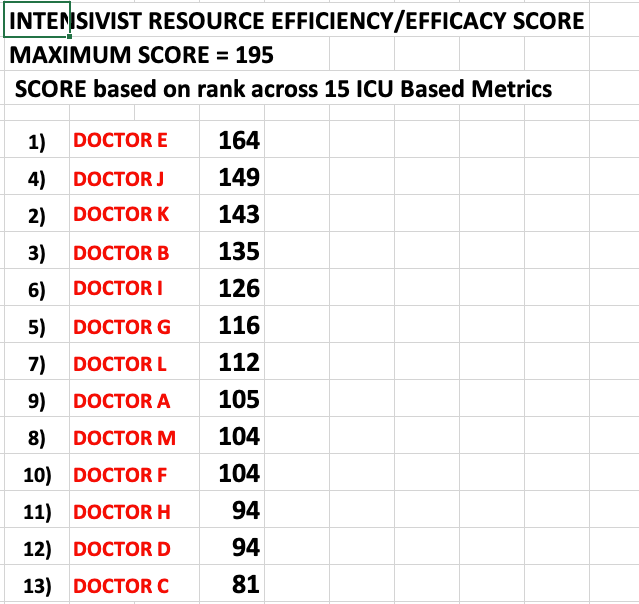
One of the best quantifications I have seen of this was a research project Pierre Kory conducted where he used his hospital’s electronic health records to evaluate all of the ICU doctors there. From it, he was able to objectively demonstrate an immense variations existed in the quality of care they provided:
As such, it makes sense to optimize who you will be working with once hospitalized (e.g., by learning through word of mouth ahead of time which hospital to send patients to). For example, during the peak of COVID, we made a point to figure out which hospitals in the area had the best results for COVID-19, so in the rare instances where we needed to send someone to the ICU, we chose the correct location.
Note: there was a huge difference in survival rates during COVID-19 depending on who managed a patient's ventilator. Unfortunately, because so many patients were initially ventilated, many of them had to be managed by individuals with limited ventilator experience, and as a result, we believe many unnecessary deaths occurred.
However, in many cases, what is much more important is not who you work with, but rather how you interact with the hospital team. Essentially, the balance that must be struck is one between ensuring the hospital staff feel outside eyes are examining what they are doing (so they are pressured to provide optimal care) but simultaneously, to not come across as confrontational or challenge the hospital staff (as in those cases, doctors will almost always double-down on what they are currently doing and refuse to cooperate with the patient’s request). Instead, seek to emotionally connect with the hospital staff so they are invested in helping the patient and feel they have a collaborative relationship with you.
Put differently, many doctors will be very reasonable if you approach them in the correct way (especially if you start the dialog early), but if it’s done in a more distraught or confrontational manner, they often will not be willing to change what they are doing. Nonetheless, it is almost impossible to get hospitals to offer things like IV vitamin C for sepsis, so if they won’t budge on it, it’s not worth starting a fight and jeopardizing your collaborative relationship with the physicians.
That said, most of us agree the single most important thing you can do if a relative is hospitalized is to be with them 24/7 as an advocate (which is one reason it’s so messed up that was not allowed during COVID-19), and in my case, despite the professional responsibilities I hold, I have taken time off that to ensure that I can effectively advocate for relatives throughout the course of their hospital stay.
Improving Hospital Care
Over the years a variety of remarkable technologies have been developed which significantly improve hospital outcomes, but due to political reasons (e.g., a desire to eliminate competition) they vanished from our hospitals. Since hospital outcomes are the area where the largest and most rapid benefit can often be detected with those forgotten therapies, I have long felt that hospital trials of them would be one of the most effective ways to positively improve the practice of medicine. In turn, once RFK announced his candidacy, a key goal here became to gradually present the therapies which I feel would be the most beneficial in the hospital setting.
For example, here, I presented a strong case ultraviolet blood irradiation would profoundly improve a wide range of hospital outcomes, here I made the case that DMSO would do the same (for a narrower set of conditions), and here I presented some of the evidence that routine IV vitamin C could dramatically reduce the death rate from sepsis (which is the number one killer in our hospitals).
However, those are just a few of the potential approaches that can be utilized. In the final part of this article (which exists an open forum for you enquire about any topics you’ve wanted to ask about such as unanswered DMSO questions) I will discuss some of the approaches (and doses for them) we believe would most benefit hospitalized patients and a few of the tricks we’ve found for identifying the best hospital and doctor to work with (assuming a word of mouth referral is not available to you).
Keep reading with a 7-day free trial
Subscribe to The Forgotten Side of Medicine to keep reading this post and get 7 days of free access to the full post archives.